Anna Pletneva interview. Anna Pletneva: “It’s very easy to build family relationships when millions want you: there’s simply nothing better for stimulating feelings! What clothes make you feel irresistible?
Lichen refers to skin diseases, the main element of which is nodular formations that cause itching, inflammation or tissue necrosis. There are several types of lichen in humans, as well as a number of reasons why it can occur, the main ones being fungal and viral infections. The course of the disease can be long, and if medical help is not sought in time, it can also be severe and dangerous for others.
Types of lichen in humans
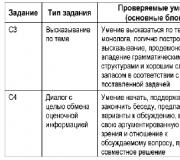
All forms of the disease have their differences. Some types are contagious, while others occur for a long time in the form of carriage with periodic relapses, which directly depends on the causative agent of the pathology. The most common forms are presented in the table.
Table: main types of lichen
Form of the disease | Pathogen | Contagiousness degree |
The form is not contagious. |
||
Or deprive Zhiber | Herpes virus | It is transmitted extremely rarely by airborne droplets. |
Shingles or herpes zoster | Herpes virus | Transmission is possible mainly to children, but is extremely rare. |
Ringworm or trichophytosis | ||
Red flat | Viruses, neurogenic factor | The disease is not transmitted. |
Disorders of biochemical processes | Not getting through. |
|
Feline ringworm | The disease is contagious. |
|
Opportunistic fungi | Not contagious. |
|
Lichen nodosum or Piedra's lichen | It is transmitted through contact and household contact. |
|
Ringworm or eczema | Systemic disorders | The disease is not transmitted. |
Shingles
Shingles (Herpes zoster) is a unilateral viral skin lesion in the form of blisters containing a clear liquid. As the disease spreads, the volume of rashes increases and, along with this, a pain syndrome occurs, which in some cases can last more than a month.
Causes
Shingles is caused by the herpes zoster virus (Varicella zoster). The main cause of infection is decreased immunity, which can be caused by a serious illness or stress. Often, shingles occurs in people who once had chickenpox and are now, having a persistent decrease in immunity, have been re-infected with this virus.
Method of infection + what it looks like in the photo
The disease is transmitted directly through contact with patients with chickenpox, through airborne droplets.
Shingles
Symptoms and signs
- rashes on the body in the form of groups of bubbles with cloudy liquid contents (see photo on the right)
- unilateral location of rashes
- the localization of the lesions corresponds to the course of the nerve trunks: on the trunk, limbs, and scalp.
- presence of itching in the areas of the rash
- temperature increase
- pain syndrome
- enlarged lymph nodes
Diagnosis of the disease
If the above symptoms appear, you must contact a specialist who, based on the clinical picture and with the help of a microscopic examination, will be able to make a diagnosis and determine the specific type of lichen. If the disease really is herpes zoster, especially its necrotic form, then a more thorough examination of the body is necessary, since it tends to develop with malignant tumors, even if their stage is very early.
Consequences
With a long course, involvement is possible nervous system with the development of postherpetic neuralgia. The disease requires hospital treatment.
Treatment and prevention
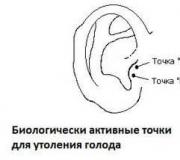
Drug treatment includes the use of antiviral drugs, such as Valtrex, Famvir or Acyclovir, which suppress the herpes virus, both in primary and secondary lesions. In addition, immunostimulating drugs, such as Isoprinosine, are also prescribed to ensure that the body itself successfully fights the disease. Since shingles is accompanied by severe pain, the doctor will also prescribe painkillers. In addition to drugs taken orally, ointments, gels and local solutions are needed - Alpizarin, Epigen, Zovirax, or interferon lotions. Since the herpes virus is killed by heat and exposure to UV rays, physiotherapy for shingles includes irradiation with a UV lamp, as well as reflexology on points that correspond to the lesions. As preventive measures, it is necessary to refrain from contact with patients with chickenpox, and if it is not possible to maintain isolation, then precautions must be taken when visiting infected people.
Pityriasis (multi-colored)
Pityriasis versicolor is a fungal infection characterized by rashes that form small, brownish spots. As a rule, their diameter is no more than 5–6 mm, and they also have the ability not to darken under sun rays, unlike healthy skin. The number of spots grows, then they merge into a single focus.
Causes of infection
The causative agent of pityriasis versicolor in humans is the fungus Pityrosporum orbiculare, which can begin to actively multiply in a humid environment - for example, when sweating. In addition, the cause of the development of this type of lichen may well be seborrheic dermatitis, especially in conditions that involve prolonged or constant exposure to high air temperatures.
Method of infecting a person
Pityriasis versicolor is not contagious and recurs only if preventive measures for its occurrence are not followed. However, recent research by scientists has proven a family predisposition to the occurrence of this disease.
 Pityriasis versicolor
Pityriasis versicolor Symptoms
- the appearance of yellow-pink spots, which then change color to a darker one
- peeling rashes
- the boundaries of the spots are uneven, but clear
- increased body sweating
Diagnostics
Pityriasis versicolor is diagnosed by a doctor using a Wood's lamp or a Balzer test performed with iodine. A specialist will also conduct a microscopic examination of the skin.
Consequences
The disease can be completely cured without any negative consequences. In chronic cases, prevention of exacerbations in the summer is especially important.
How and with what to treat
Antifungal agents are used as treatment with medications: Fungoterbin, Nizoral or Mycozoral. All of them are used externally, since pityriasis versicolor only affects surface layer skin. Oral medications are also prescribed: Fluconazole, Ketoconazole. As a rule, it is not difficult for a medical specialist to cure the disease, although the characteristic pigmentation may remain for some time. As a preventive measure, people (especially men) with excessive sweating or seborrheic dermatitis should be given Special attention disinfect your clothes and keep them clean.
Pink (lichen Zhibera)
Pityriasis rosea consists of large spots that have a pinkish tint. The disease occurs mainly in adolescents and can last for several weeks or several months.
Causes
The disease presumably has a viral etiology, although until now there is no exact data on which virus causes pityriasis rosea in humans. Most scientists agree that this is due to certain types of herpes, which are activated when the immune system is weakened.
Method of infection + photo of skin
Pityriasis rosea is not contagious and is not transmitted by airborne droplets, household contact, or sexual contact.

Symptoms
- the appearance of round spots that begin to peel off in the middle
- rashes with a red border around the periphery
- unlike other forms of lichen, the rashes do not merge into a single lesion
- slight pain
Diagnosis of the disease
A specialist can diagnose the disease by examining a person using a microscope and conducting serological tests to detect syphilis in the patient, the rashes of which have a clinical picture similar to lichen.
Consequences
After healing, an area with disturbed pigmentation forms at the site of the lesion.
How can you cure
In many cases, the disease can go away on its own and does not require special treatment. However, serological tests are still necessary to find out the real reason appearance of rashes. To alleviate the condition, the doctor may advise eliminating underwear made from synthetic and woolen materials from your wardrobe. Drugs are usually limited to the prescription of Ascorutin or antihistamines. As a preventive measure for pityriasis rosea, persons with reduced immunity in the autumn and spring require additional vitamins and immunostimulating drugs.
Shearer
Ringworm in humans can affect both the hairy parts of the body and smooth skin. The second name for this disease is microsporia. It can be severe and affects mainly children preschool age. The incubation period, depending on the type of microsporia, ranges from 5 days to several weeks.
Why did it appear on the skin of a child or adult?
The disease is caused by fungi of the genus Microsporum and Trichophyton, which begin to actively reproduce in warm and humid places.
Method of infection
The disease is highly contagious and is easily transmitted from person to person, as well as from animal to person. Moreover, if the infection came from an animal, then the disease, as a rule, occurs in a more severe form. In addition, you can become infected with the ringworm fungus even when cultivating the soil without gloves. The method of transmission of the virus is through household contact.
Symptoms + photos
 Ringworm
Ringworm - formation of spotty reddish rashes (photo on the right)
- peeling
- if the focus of the disease is located on the scalp, then you can notice that the hair breaks at the root in this place.
- lesions tend to grow
- in some advanced cases, a sweetish odor emanates from the spots
Diagnosis
To diagnose ringworm, it is advisable to contact a dermatologist who examines samples of the affected skin tissue under a microscope, and will also be able to make an accurate diagnosis during a visual examination of the patient based on the clinical picture. In addition, diagnostics can be carried out using the yellow-green glow of a Wood's lamp. A photo of ringworm in humans is shown on the right.
Consequences
The pathology can be completely cured, but in its absence it can become chronic. A dangerous complication is the formation of abscesses.
Treatment and prevention
Since the causative agent of ringworm is a fungus, it is advisable to take antifungal drugs as medicinal treatment: Lamisil, Fungoterbin. If the skin lesion is shallow, then you can only get by with local ointments, using, for example, “Mycozoral” or a weak solution of iodine, or sulfur ointment. If the focus of the disease has spread to the deeper layers of the skin, then solutions and ointments must be combined with antifungal drugs that are taken orally. It is impossible to determine on your own the extent of ringworm damage, so it is important to consult a doctor to prescribe the correct treatment. In the treatment of this disease, physiotherapy also plays an important role: irradiation with a UV lamp, phonophoresis and electrophoresis will significantly speed up the fight against the fungus and help eliminate unpleasant symptoms in the affected areas. As a preventive measure, you should avoid using other people's personal hygiene products and contact with infected people and animals.
Lichen planus is a disease that can occur at any age, is characterized by a rather protracted course and consists of red papules with a shiny surface. The rash may form rings or certain lines on the surface of the skin.
Causes
Like psoriasis, lichen planus has autoimmune causes. For it to appear, the patient, as a rule, must have a genetic predisposition and a certain provoking factor, which may well have a psychological etiology, or may be an allergic reaction.
How can you get infected?
This disease is not contagious and cannot be transmitted from a sick person to a healthy person.

Symptoms and signs
- the appearance of reddish papules
- long-term preservation of pigmentation even after resorption of papules
- localization on back side feet, legs, and also, in some cases, along the nerve
- damage to the mucous membranes
- painful sensations in the areas of the rash
Diagnostics
Diagnosing the disease by a dermatologist is usually not difficult. Papules have characteristic appearance, inherent only this type depriving, and the presence of a Wickham mesh only confirms the diagnosis. However, a specialist may prescribe additional examinations in order to identify or exclude other serious diseases of the body that may accompany lichen planus.
Consequences
Lichen ruber does not cause serious consequences if the provoking factors are promptly eliminated. Some of its forms, such as warty, cystic and ulcerative, are difficult to cure.
How and what to treat
Antihistamines, vitamins (especially A and C), as well as drugs that have a sedative effect are widely used as treatment. In addition, the use of external medications is indicated to reduce the discomfort caused by the formation of lichen planus. In particular, such agents can be talc or even ordinary starch. Since the disease is autoimmune in nature, certain preventive measures to prevent it have not yet been developed. If any type of lichen occurs, you should not self-medicate in order to avoid the transition of the initial stages of the disease to more advanced ones. The dosage of the drugs listed above can only be determined by the attending physician.
Lichen squamosus (psoriasis)
An equally common name for scaly lichen in humans is psoriasis. The disease is chronic in nature, characterized by a latent course, combined with relapses. Psoriasis rashes are prone to inflammation and are located mainly on the outer side of the extensor surface.
Causes
The causes of psoriasis can be immunological changes in the human body, often genetically programmed. In such cases, various stressful situations can provoke the occurrence of psoriasis.
Method of infection
The disease is not contagious, since its etiology suggests an autoimmune nature of the disease.
 Lichen squamosus (psoriasis)
Lichen squamosus (psoriasis) Symptoms
- the appearance of raised spots above the skin that have a reddish color
- the rashes are very dry, so they provoke severe itching
- The typical location of lichen planus is the folds of the arms, legs, buttock and lumbar regions.
- the tendency of spotty rashes to increase in diameter and merge into large lesions
Diagnostics
Based on general clinical picture, a dermatologist will usually easily determine the type of disease and the degree of its intensity. In addition to a visual examination, the patient may be prescribed a blood test, the results of which will be considered as a confirmatory factor in the presence of psoriasis. In some cases, histology is indicated to examine the affected skin tissue for malignant cells.
Consequences
The disease occurs in a chronic form with periods of relapse. The pustular form can provoke intoxication of the body.
Treatment and prevention of the disease
In order for the treatment tactics to be correct, it is necessary to rely on the patient’s age, gender, concomitant diseases, as well as the nature of the course of psoriasis. Drug treatment of psoriasis involves ointments, gels and solutions that have a local effect: “Tazarotene”, “Dithranol”, and care must be taken in their use, since such ointments cannot be applied to too large areas of the affected skin. In some cases, treatment with certain types of antibiotics (Clarithromycin or Erythromycin) may be used. In general, due to the fact that the pathogenesis of psoriasis has not yet been sufficiently studied, methods for its treatment are still at the stage of research and experimentation. Since lichen squamosus is an autoimmune disease rather than a viral one, as a preventative measure for people with a genetic predisposition to it it is necessary to avoid stress, overwork and serious psychological trauma.
Feline ringworm
Feline ringworm is contagious and is most often transmitted from small kittens, which is where it gets its name. Characterized by the formation of spots with a clear boundary. Treatment requires careful laboratory diagnosis.
Causes
Method of infection
The disease is highly contagious and is transmitted through direct contact with an animal or through the use of contaminated objects. Damage is especially common in children and adolescents.
Symptoms
With feline lichen, the scalp, skin of the arms, palms, face, and buttocks are affected. The first signs are observed a couple of weeks after contact, and are characterized by the formation of redness in the form of a ring. When localized in the scalp area, fragility of the hair at its base is noted.
The spots tend to merge to form formations with a diameter of 7 cm. Itching and peeling are noted. In the absence of timely treatment, blisters and suppuration appear.
Diagnostics
To make a diagnosis, a scraping from the affected area is examined to determine the type of fungus.
Treatment
Therapy is aimed at preventing the spread of the fungus to healthy tissue. To do this, the hair is cut, and this must be done every week until complete healing. The affected areas are treated with iodine and antifungal ointment. Clotrimazole, Mycoseptin, Ketonazole and so on are considered effective. The course may take several weeks.
Consequences
If the scalp is affected, baldness or disruption of uniform hair growth may occur.
The formation of flaky spots after intense tanning is a sign of sunburn. This is a dermatological disease of a fungal nature. The outbreak occurs in the spring and autumn.
Causes
The main cause of pathology is fungi. They are classified as opportunistic, that is, in the absence of provoking factors, they are constantly on human skin and do not cause any abnormalities. The fungus is activated after intense exposure sunlight. Also provoking factors are heart pathologies, endocrine disorders, gastrointestinal diseases and frequent colds.
Method of infection
Considering the type of pathogen, we can say with confidence that the pathology is not contagious. Carriage of the pathogen does not manifest itself in any way and is considered as the norm.
 Intense sunbathing can lead to sunburn
Intense sunbathing can lead to sunburn Symptoms
Solar lichen appears as asymmetrically shaped spots of coffee-milk color. The spots tend to merge; subsequently they do not perceive tanning and become especially noticeable. Itching and flaking are possible. Any part of the body can be affected; in children, the scalp is often involved.
Pathology occurs in three stages:
- Formation of pink spots.
- Darkening of spots and their combination.
- Covering spots with scales.
Diagnostics
To diagnose, it is enough to conduct an examination. Ringworm is confirmed using an iodine test and scraping.
Treatment
Treatment is prescribed by a doctor after confirming the diagnosis. Salicylic ointment, Mycozolon, sulfur ointment are used. It is optimal to use ointments and sprays for uniform application. Antifungal agents are used several times a day. The total duration of therapy is 14 days. As a supplement, drugs in the form of tablets for oral administration can be used.
Consequences
The pathology does not cause any consequences, but if preventive measures in the form of limiting sunbathing are not followed, the appearance of large quantity stains, which negatively affects the appearance.
Each form of pathology has its own treatment characteristics based on the pathogen. Along with traditional drugs, folk treatment is also used. The following remedies are especially often used for lichen:
- Tar soap. It can be used for daily hygiene procedures. A little tar is suitable for compresses.
- Iodine. The prepared solution is used to treat lesions. Can be alternated with brilliant green.
- Solid oil. It is used to lubricate lesions until complete healing.
- Egg. To treat the outbreak, liquid is used that accumulates between the shell and the film inside the egg.
- Vinegar. Apple cider vinegar is most often used. You should take 0.5 liters of solution and 3-4 cloves of garlic. The garlic is crushed and mixed with vinegar. The resulting solution is used for compresses.
- Tea tree oil. The lesion is treated with a mixture of oil and water in a ratio of 1:4. You can also use a mixture of olive oil and tea tree oil in a ratio of 10:1. Used up to 5 times a day.
Diet
As with any other disease, with lichen it is important to follow some dietary rules to speed up recovery. The main requirements will be:
- Increasing the amount of water to remove toxins.
- Consuming grains to cleanse the intestines.
- Consumption of dairy products to normalize intestinal flora.
- Eating 4-5 times a day.
You will have to give up spices, alcohol, marinades and pickles. During exacerbations, you should reduce the consumption of fatty and spicy foods, as well as large amounts of baked goods.
Infectious skin diseases are not always easy to recognize, especially in initial stage. Pityriasis rosea in humans is a complex ailment that has not been fully studied by doctors. The problem is solvable and the symptoms can be eliminated by knowing the characteristic features of the disease.
Pityriasis rosea or Zhiber's pink pityriasis refers to skin irritation in the form of elongated red spots caused by infection. The rash is similar to the manifestations of allergic reactions. Experts classify this disease as a type of dermatosis and argue that lichen may be of viral origin.
People aged 10-35 years are most susceptible to the disease; in total, the risk of infection persists up to 55 years.
Skin rashes heal within 1-3 months, in in rare cases Ringworm lasts longer.
The rash begins to develop after the first spot appears on the skin (diameter is about 2 cm or more). Then, yellowing of the skin, dryness, and peeling are observed in the affected area. Pityriasis rosea not considered a contagious disease, although doctors have not reached a consensus on this matter.
Some dermatologists claim that the causative agent of infection is transmitted by airborne droplets.
Basically, the disease appears after suffering from colds and infectious diseases. The spots on the skin are covered at the edges with a thin border consisting of scales.
Causes
 The cause of Pityriasis rosea may be complication after ARVI, a consequence of disturbances in the functioning of the immune system. Doctors draw an analogy with herpes type 6, but so far the pathogen is not exactly known. There are factors that increase the risk of developing lichen.
The cause of Pityriasis rosea may be complication after ARVI, a consequence of disturbances in the functioning of the immune system. Doctors draw an analogy with herpes type 6, but so far the pathogen is not exactly known. There are factors that increase the risk of developing lichen.
These are the following health problems:
- intestinal disorders
- nervous breakdown, stress
- metabolic disorders
- hypothermia
- oncological diseases
Pityriasis rosea may appear after insect bite(there are known cases where fleas, lice and bedbugs caused a characteristic rash in humans).
Another possible reason is seasonal outbreaks, since in the fall and spring the immunity of many is weakened and unstable to diseases. Vaccination is also considered a factor that can trigger the development of the disease.
Symptoms of pityriasis rosea

In the initial stage, the disease may proceed unnoticed. Possible appearance slight itching, which intensifies after physical work or stress. In some people, pityriasis rosea is accompanied pain in muscles, joints, migraines.
Symptoms may resemble those of ARVI - dizziness, weakness, fever, loss of appetite, rhinitis (runny nose), sore throat.
The spots gradually begin to spread throughout the body, except the face, neck and limbs. In rare cases, the rash spreads to the hands and feet.
Over time, the spots become crusty along the contour, swell and darken. It is important not to confuse the rash that appears with a common allergy and do not self-medicate. After the first reddish spot appears, the rest do not appear immediately, but after 1-2 weeks.
A convex formation, which has an oval shape and a color characteristic of lichen, should alert the patient.
Diagnostics
The first thing the doctor should do is examine the patient. Preliminary diagnosis is based on recognition of symptoms by appearance skin, rash features.
Then the patient is taken scraping for analysis and do a rapid test for the presence of fungi in the body. Such procedures are performed by a dermatologist at a skin and venereal disease clinic.
Pityriasis rosea is sometimes confused with other diseases (for example, secondary syphilis, or), so additional tests are prescribed if necessary. The patient may be referred for a skin biopsy, blood donation, urine donation and other procedures. The doctor must fully examine the patient to establish a clear diagnosis and make sure that the rash is caused by pityriasis rosea.
How to treat pityriasis rosea
There are no special treatment methods for Lichen Rosea; under normal conditions, it disappears after a couple of months. Medical intervention is required if the disease takes on atypical forms.
Bubble, a confluent or pinpoint rash is considered a pathology.
A complication is also considered ring-shaped lichen, in which the spots reach a diameter of 8 cm. In this case, the disease may not go away for a long time.
Treatment is based on the results of the examination and in accordance with the patient’s health condition. In especially severe cases, when the spots greatly increase and spread to new areas of the body, the doctor prescribes antibiotics (Erythromycin, Tetracycline).
Additional measures:
- From the diet excluded citruses, nuts, eggs, some fruits (red), alcoholic drinks, tea, chocolate, coffee, spicy dishes.
- During illness Not recommended use soap and a washcloth; only shower with water is allowed.
- Women You can't wear makeup for 3-5 weeks until the lichen goes away.
- Doctors Patients are not advised to sunbathe and wear underwear made from synthetics.
If necessary, the doctor can prescribe it to the patient.
For example:
- Suprastin
- Claritin
- Tavegil
- Erius
- Xizal
- Loratadine
Treatment can also be carried out using corticosteroids:
- Hydrocortisone
- Clobetasol
- Diprospan
Treatment should be carried out under conditions in which water procedures are excluded or reduced to a minimum. Useful for strengthening immunity during illness take vitamins.
Exist traditional methods treatments for pityriasis rosea, but they should be treated with caution and all questions should be discussed with your doctor.
In most cases, the disease goes away within 8 weeks, but there are exceptions. It is important to approach the issue responsibly, consult a doctor about everything, and follow preventive measures after recovery.
Ringworm - this concept unites a wide group of skin diseases that can have different nature occurrence, but similar manifestations (rashes, itching). Based on these characteristic symptoms, one can confidently diagnose lichen, but determining the degree of its contagiousness and understanding what type of infection we are dealing with is much more difficult. However, an accurate diagnosis is necessary; the treatment method and ways to eliminate the problem depend on this.
The causative agents of lichen are a variety of pathogenic fungi; in some cases, the disease is of a viral nature, and the impetus for its development is a weakened immune system. In any case, every person needs to know what lichen looks like at the initial stage in order to promptly seek medical help. Coping with skin diseases is not easy, so the sooner treatment is started, the higher the chance of a full recovery.

The course of lichen can be varied and largely depends on its type. In some patients, gradual damage to the skin can be observed, in others, rashes appear throughout the body in a short period of time. The disease can affect any part of the body, from the scalp to the genitals. Most often, the causative agents of lichen are microscopic fungi, which are conventionally divided into three large groups:
- Anthropophilic. They only affect people and are transmitted through contact with a carrier and through the use of common household items.
- Zoanthropophilic. They are found not only in humans, but also in animals. Animal lovers and children most often suffer from this type of lichen.
- Geophilic. Infection occurs through contact with the ground, and is more common among people performing agricultural work.
In other cases, the development of lichen is caused by a virus that is present in the body of most people, but is activated and manifests itself as skin rashes only under favorable circumstances (decreased immunity, hypothermia, stress, serious illnesses).
Despite the variety of pathogens, skin diseases at the initial stage share common symptoms:
- Inflammatory processes on the skin.
- Characteristic rashes with clearly defined boundaries separating the affected skin from healthy skin.
- Changes in pigmentation in the lesions.
- Intense itching, irritation
- Dryness and flaking of the skin
Therapy should be started at the first signs of the disease, since the initial stage of lichen is easier to treat. If the process of skin damage is not stopped in time, then the disease will progress to an advanced stage. With this development of events, the infection can spread throughout the body and result in a secondary infection and other serious complications.
What does lichen look like at the initial stage in humans (photo)?
Some varieties of lichen are extremely contagious, so if infected, it is necessary to minimize contact with others and remain in isolation for some time. Contagious infections include: ringworm, shingles and pityriasis rosea. When the diagnosis is confirmed, the patient is transferred to a home regime or placed in a hospital; until complete recovery, the circle of contacts is limited, and individual dishes, household items and personal hygiene products are allocated.
Let's take a closer look at the most common types of lichen and tell you about them. distinctive features and treatment methods.

Trichophytosis of smooth skin appears on open areas of the body: on the upper and lower extremities, neck, face, and less often on the torso. The rash looks like red-pink spots with a clear border. The skin in the affected area is swollen, flaky, covered with small vesicles, which, as they mature, burst and become crusty. This process is accompanied by severe itching. As they regress, such spots turn into rings with a clearly defined boundary.
 Pityriasis rosea (lichen of Zhibera). This is a skin disease of a viral nature, the causative agent of which has not yet been fully studied. The initial stage of pityriasis rosea manifests itself by the appearance of a “maternal plaque”, which looks like a red spot with a diameter of 2 to 5 cm. After some time, general malaise is noted and pink spots appear throughout the body, the center of which is much paler than the edges. Along the periphery of such rashes, peeling is observed, accompanied by mild itching. The development of the disease is associated with seasonal decreases in immunity (spring and autumn).
Pityriasis rosea (lichen of Zhibera). This is a skin disease of a viral nature, the causative agent of which has not yet been fully studied. The initial stage of pityriasis rosea manifests itself by the appearance of a “maternal plaque”, which looks like a red spot with a diameter of 2 to 5 cm. After some time, general malaise is noted and pink spots appear throughout the body, the center of which is much paler than the edges. Along the periphery of such rashes, peeling is observed, accompanied by mild itching. The development of the disease is associated with seasonal decreases in immunity (spring and autumn). Shingles. It is caused by the varicella zoster virus, which, after chickenpox in childhood, remains in the body in a “dormant” state and is activated under the influence of factors unfavorable to the body (hypothermia, chronic diseases, decreased immunity). The initial stage of herpes zoster is accompanied by a deterioration in general health. The symptoms resemble those of colds. General weakness appears, febrile conditions occur with increased temperature, chills, muscle pain, and enlarged lymph nodes. Simultaneously with these manifestations, burning and itching are noted at the sites where the virus moves through the nerve cells. Most often, the area of localization of lichen chooses the intercostal nerves; the process is usually unilateral. Red, inflamed spots appear at the site of the lesion, on which blisters filled with clear liquid form within 3-4 days. Their formation is accompanied by pain, burning and itching. After some time, the blisters open, crust over, dry out and fall off, leaving behind spots of hyperpigmentation. Pain syndrome with herpes zoster can persist for a long time.
Shingles. It is caused by the varicella zoster virus, which, after chickenpox in childhood, remains in the body in a “dormant” state and is activated under the influence of factors unfavorable to the body (hypothermia, chronic diseases, decreased immunity). The initial stage of herpes zoster is accompanied by a deterioration in general health. The symptoms resemble those of colds. General weakness appears, febrile conditions occur with increased temperature, chills, muscle pain, and enlarged lymph nodes. Simultaneously with these manifestations, burning and itching are noted at the sites where the virus moves through the nerve cells. Most often, the area of localization of lichen chooses the intercostal nerves; the process is usually unilateral. Red, inflamed spots appear at the site of the lesion, on which blisters filled with clear liquid form within 3-4 days. Their formation is accompanied by pain, burning and itching. After some time, the blisters open, crust over, dry out and fall off, leaving behind spots of hyperpigmentation. Pain syndrome with herpes zoster can persist for a long time. Variegated (pityriasis versicolor). It is caused by the yeast-like fungus Pityrosporum, which, multiplying in the stratum corneum, affects the cells of the epidermis, causing pigmentation disorders. Appears as small spots various shapes, different in color from healthy skin. They may be paler than the main background of the epidermis, or, on the contrary, much darker. The spots tend to merge and form large scaly lesions. The main location of lichen is the chest, back and neck. As spots form, the patient becomes concerned increased sweating and mild itching. This type of lichen is not contagious; the mechanism of its appearance is associated with genetic predisposition and a combination of hormonal and immune disorders. Spots of pityriasis versicolor become especially noticeable on untanned skin in the summer, so this disease has another name - “Sun fungus”.
Variegated (pityriasis versicolor). It is caused by the yeast-like fungus Pityrosporum, which, multiplying in the stratum corneum, affects the cells of the epidermis, causing pigmentation disorders. Appears as small spots various shapes, different in color from healthy skin. They may be paler than the main background of the epidermis, or, on the contrary, much darker. The spots tend to merge and form large scaly lesions. The main location of lichen is the chest, back and neck. As spots form, the patient becomes concerned increased sweating and mild itching. This type of lichen is not contagious; the mechanism of its appearance is associated with genetic predisposition and a combination of hormonal and immune disorders. Spots of pityriasis versicolor become especially noticeable on untanned skin in the summer, so this disease has another name - “Sun fungus”. Lichen planus. The disease has not been fully studied; doctors suggest that this type of lichen is caused by a virus and occurs against the background of immune system disorders, allergies or severe stress. Ringworm is not considered contagious. Multiple rashes look like red or purple flat nodules that appear on the skin or mucous membranes. Their appearance is accompanied by intense itching. As the disease progresses, the nodules merge into plaques with a mesh pattern. Most often, this type of lichen affects middle-aged and elderly women. The rashes can have different shapes and look like warts, rings, erythematous tubercles or erosions.
Lichen planus. The disease has not been fully studied; doctors suggest that this type of lichen is caused by a virus and occurs against the background of immune system disorders, allergies or severe stress. Ringworm is not considered contagious. Multiple rashes look like red or purple flat nodules that appear on the skin or mucous membranes. Their appearance is accompanied by intense itching. As the disease progresses, the nodules merge into plaques with a mesh pattern. Most often, this type of lichen affects middle-aged and elderly women. The rashes can have different shapes and look like warts, rings, erythematous tubercles or erosions. Psoriasis (scaly lichen). It is considered a non-contagious disease of an autoimmune nature, in the occurrence of which genetic predisposition plays a major role. This skin disease is still considered incurable. A characteristic symptom of psoriasis is red, dry spots covered with grayish scales that protrude above the surface of the skin. Small spots can merge into fairly large, dense plaques. Skin elements do not have a specific localization and can appear on any part of the body. Patients with psoriasis note a general deterioration of their condition, weakness, constant discomfort and incessant itching.
Psoriasis (scaly lichen). It is considered a non-contagious disease of an autoimmune nature, in the occurrence of which genetic predisposition plays a major role. This skin disease is still considered incurable. A characteristic symptom of psoriasis is red, dry spots covered with grayish scales that protrude above the surface of the skin. Small spots can merge into fairly large, dense plaques. Skin elements do not have a specific localization and can appear on any part of the body. Patients with psoriasis note a general deterioration of their condition, weakness, constant discomfort and incessant itching.
Treatment methods
When the first symptoms of lichen appear on the body, you should immediately contact a dermatologist for examination and treatment. At the initial stage, the disease is treated much easier and faster. Let us dwell in more detail on the methods of treatment of each type of lichen:
Ringworm
 How to treat ringworm at the initial stage, will be determined individually by a dermatologist. The treatment regimen will largely depend on the location of the lesions. If lichen appears on the scalp, then the affected areas are treated with local antifungal agents: ointments and creams Miconazole, Terbinafine, Clotrimazole. Hair is washed twice a week with special medicated shampoos (Nizoral, Dermazol).
How to treat ringworm at the initial stage, will be determined individually by a dermatologist. The treatment regimen will largely depend on the location of the lesions. If lichen appears on the scalp, then the affected areas are treated with local antifungal agents: ointments and creams Miconazole, Terbinafine, Clotrimazole. Hair is washed twice a week with special medicated shampoos (Nizoral, Dermazol).
To treat smooth skin affected by lichen, ointments with tolnaftate and terbinafine are used. In addition, in the morning the rashes are treated with iodine, and in the evening sulfur-tar or sulfur-salicylic ointment is applied. If multiple rashes appear on the body, the doctor will prescribe a drug in tablets for oral administration (Griseofulvin). Since ringworm is very contagious, the patient is isolated for the entire duration of treatment.
Folk remedies
When treating ringworm, in addition to medicinal methods, you can use traditional medicine:

Pityriasis rosea
 Pityriasis rosea does not require special treatment; in most cases it goes away on its own within 4-6 weeks. The doctor may prescribe antihistamines (Zyrtec, Loratadine, Suprastin), they will help get rid of itching. To maintain immunity, it is recommended to take immunomodulators and vitamin-mineral complexes. To eliminate flaking and soften the skin, you can use natural oils (peach, almond, sea buckthorn) or non-hormonal creams. It is better not to use products containing salicylic acid or sulfur, as they greatly dry out the skin. During treatment, it is not recommended to be in the sun or indulge in water procedures.
Pityriasis rosea does not require special treatment; in most cases it goes away on its own within 4-6 weeks. The doctor may prescribe antihistamines (Zyrtec, Loratadine, Suprastin), they will help get rid of itching. To maintain immunity, it is recommended to take immunomodulators and vitamin-mineral complexes. To eliminate flaking and soften the skin, you can use natural oils (peach, almond, sea buckthorn) or non-hormonal creams. It is better not to use products containing salicylic acid or sulfur, as they greatly dry out the skin. During treatment, it is not recommended to be in the sun or indulge in water procedures.
Folk remedies
 At home, pityriasis rosea can be treated with a homemade calendula-based composition. To do this, dry calendula flowers are crushed and mixed with petroleum jelly in a ratio of 1:5. The resulting mixture is well ground until smooth and lubricates the rashes on the skin. Procedures can be done daily, before bedtime. The medicinal composition should be stored in the refrigerator.
At home, pityriasis rosea can be treated with a homemade calendula-based composition. To do this, dry calendula flowers are crushed and mixed with petroleum jelly in a ratio of 1:5. The resulting mixture is well ground until smooth and lubricates the rashes on the skin. Procedures can be done daily, before bedtime. The medicinal composition should be stored in the refrigerator.
Shingles
Since this type of lichen is viral in nature, the disease is treated with antiviral drugs (Acyclovir, Valacyclavir). In case of severe pain, analgesics are prescribed for oral administration or an anesthetic gel with lidocaine for external use. The onset of the disease is usually accompanied by a deterioration in health and an increase in temperature, so the patient is recommended to take Paracetamol or other anti-inflammatory drugs (Ibuprofen). In some cases, if complications arise, antibiotic therapy may be necessary.
Folk remedies
Shingles, in addition to the main methods of therapy, can be treated with traditional methods:

Pityriasis versicolor
Pityriasis versicolor is caused by a fungus, therefore it is treated with local antifungal drugs in the form of ointments, gels, creams, lotions, and sprays. If necessary, the patient is prescribed antimycotic drugs in tablets or capsules (Ketoconazole, Terbinafine). Part of antifungal therapy is tanning. In the summer, a patient with pityriasis versicolor is recommended to be in the sun more often, as ultraviolet rays help destroy the fungus.
Folk recipes

Lichen planus
To eliminate painful itching in lichen planus, antihistamines (Tavegil, Claritin, Suprastin) are used, skin manifestations are combated with hormone-based corticosteroid ointments, and solutions and mixtures with menthol and citric acid are used. If the disease progresses, antibiotics (macrolides, tetracycline) are used. A course of vitamin therapy (based on vitamin A) helps to alleviate the condition; such treatment normalizes metabolic processes and regulates the division of skin cells.
Folk recipes
- In case of damage to the oral mucosa ethnoscience advises using sea buckthorn oil to treat rashes. For quick healing, apply applications with sea buckthorn oil, applying them to the affected areas of the mucous membrane for 20-30 minutes.
- On the skin, lichen planus can be treated apple cider vinegar. To do this, it is enough to wipe the rash with undiluted vinegar 4 to 6 times a day.
Psoriasis
 Lichen squamosus is non-contagious and does not require isolation of the patient, but is considered incurable disease. The course of therapy is aimed at eliminating external symptoms and prolonging the period of remission. For this purpose, hormonal ointments (Cloveit, Skincap) and a special set of therapeutic measures are used, based on general cleansing of the body, strengthening the immune system and general health.
Lichen squamosus is non-contagious and does not require isolation of the patient, but is considered incurable disease. The course of therapy is aimed at eliminating external symptoms and prolonging the period of remission. For this purpose, hormonal ointments (Cloveit, Skincap) and a special set of therapeutic measures are used, based on general cleansing of the body, strengthening the immune system and general health.
Folk remedies
In addition to drug therapy at home, you can use a variety of herbal preparations, on the basis of which tinctures, extracts and decoctions are prepared for oral administration. Baths with sea salt, celandine, string, soda, and oat decoction give a good effect, which help improve the condition and reduce the severity of unpleasant symptoms.
– a group of infectious dermatoses of a fungal or viral nature, occurring with rashes, itching, peeling, impaired skin pigmentation, and hair loss. Children have different kinds lichen (ringworm, multicolored, red flat, pityriasis versicolor, shingles), having specific manifestations. To identify lichen in children, dermatological diagnostics are performed: examination of the skin under a Wood's lamp, microscopy of scrapings, virological and cultural examination. Treatment of lichen in children includes quarantine measures, treatment of affected skin areas with antifungal, antiviral, corticosteroid drugs, and physiotherapy.
Lichen planus in children
This type of lichen in children is extremely rare. The disease affects the skin, mucous membranes, and rarely the nails. Dermatosis is characterized by a monomorphic rash in the form of flat nodules of bright red or bluish color with a shiny surface, 2–3 mm in diameter. Lichen planus is accompanied by intense itching, depriving children of sleep. Merging, the nodules form small plaques with small scales on their surface.
The typical localization of rashes with lichen planus in children is the flexor surfaces of the forearms, wrist joints, internal surfaces thighs, groin and axillary areas, mucous membranes of the mouth.
Shingles in children
Shingles (herpes) develops in children over 10 years of age and adults who have had chickenpox in the past. The appearance of skin rashes with shingles in children is preceded by a flu-like condition - malaise, chills, fever, burning sensation, numbness or tingling along the sensory nerves, in the area of future rashes.
After 1-2 days, groups of 0.3-0.5 cm vesicles filled with transparent contents appear on an erythematous-edematous background. The rash is located linearly, along large nerve trunks and nerve branches. During the period of active rashes, high fever, radiating pain along the intercostal and trigeminal nerves, and lymphadenitis are noted. After a few days, the contents of the bubbles become cloudy and dry out; In their place, crusts form, which then fall off, leaving behind light pigmentation. Recovery usually occurs within 15 days to 1 month.
With herpes zoster, children may develop stomatitis, conjunctivitis, keratitis, iridocyclitis, optic and oculomotor neuritis, and neuralgia. In weakened children, herpes zoster can be complicated by serous meningitis, encephalitis, and myelitis.
Diagnosis of lichen in children
Diagnosis of lichen in children, as well as determination of its form, is carried out by a pediatric dermatologist, mycologist or infectious disease specialist. To confirm the expected diagnosis, the doctor conducts a visual examination of the skin, special tests, and fluorescent diagnostics. Each form of lichen in children has its own characteristics of the morphology of the elements, as well as the characteristic fluorescence of the affected areas with rubella), vitiligo, alopecia areata in children (with ringworm).
Treatment of lichen in children
The treatment regimen for lichen in children depends on the type of infection and the severity of the manifestations. In all cases, treatment should be carried out under the supervision of a dermatologist. Contagious forms of lichen require isolation of the sick child and temporary cessation of contact with other children.
Treatment of lichen in children caused by fungal pathogens involves shaving the hair in the affected area, taking systemic antimycotics (griseofulvin), treating the skin with antifungal ointments, carrying out restorative vitamin therapy, and immunomodulatory therapy. For severe itching of the skin, antihistamines and corticosteroid ointments are prescribed. In case of damage to the flexible scalp, medicated fungicidal shampoos are used. The criterion for cure for fungal lichens in children is a three-fold negative test for fungi.
Treatment of herpes zoster in children is carried out with local and general action(interferon, acyclovir), analgesics, NSAIDs. The areas of rash are lubricated with brilliant green and other disinfectant solutions to prevent suppurative complications. Physiotherapeutic procedures are very effective for herpes zoster in children - solux, ultraviolet irradiation, ultrasound therapy, electrophoresis, diathermy, magnetic field. In cases of severe pain, novocaine blockades and reflexology are performed.
An important point is strict adherence to hygiene rules (regular change of the child’s linen and clothes, washing and ironing them; avoidance of combing items; disinfection of personal hygiene items), temporary exclusion of common water procedures, hypoallergenic food.
Prevention of lichen in children
Factors to prevent lichen infection are: complete isolation sick child from healthy children; limiting contacts of children with stray animals; Regular examination of pets by a veterinarian. It is extremely important to pay attention to strengthening children’s immunity and instilling hygiene skills in children.
Treatment of lichen in children is a long and patient process. Often, the disappearance of visible manifestations does not mean complete recovery, therefore it is necessary to strictly adhere to the terms of therapy and quarantine indicated by the doctor.